Depression In Women

Depression is a serious mental health condition that affects 23% of adults (60 million people) in the U.S. each year. While women are more likely than men to seek treatment, feelings of embarrassment and shame may still keep them from considering counseling.
At least half of women cite denial as a barrier to treatment. It is important to remember that depression is a treatable condition - and it can occur in any woman, at any time, and for various reasons regardless of age, race or income.
- Approximately 24% of women in the U.S. currently live with depression.
- Over one-third of women (36.7%) report having been diagnosed with depression in their lifetime compared with 20.4% of men.
- Black, Hispanic, and Asian American women experience more depressive symptoms, on average, than any other population subgroup.
- Many biological factors may contribute to depression in women, such as family history, the way your body’s cells communicate, hormones, and other health problems.
- Social factors may also lead to higher rates of clinical depression among women, including stress from family responsibilities and increased rates of sexual abuse, domestic abuse, and poverty.
- Approximately 10%-20% of all new mothers experience postpartum depression, which most frequently occurs within the first year after the birth of a child.
- According to data from MHA’s screening tool, women who took the postpartum depression screen reported feelings of inadequacy as a mother, fear of losing their children to Child Protective Services (CPS), and overwhelm due to a lack of support.
- Learn more about pregnancy and postpartum disorders.
- Perimenopausal depression is highly prevalent in women during the transition to menopause. When women are in perimenopause, or the period of time before menopause, estrogen and progesterone levels drop. So do serotonin, dopamine, and GABA levels, the body’s “feel-good” chemical messengers. This hormonal change can cause women to feel symptoms of depression.
- On average, women in the U.S. reach menopause at age 52.
- There is a high rate of suicide in women between 45-54 years old. This may be due to the biological changes that come with the transition to menopause and is important for medical professionals to be aware of.
- Some symptoms of perimenopausal depression include:
- extreme feelings of irritability
- anxiety
- paranoia
- loss of enjoyment
- low energy
- difficulty with memory and concentration
- decreased sexual interest
- decreased self-esteem
- Research shows a strong relationship between eating disorders (anorexia and bulimia nervosa) and depression in women. The typical age of onset for eating disorders in women is between 16-25. However, many middle-aged women also experience eating disorders.
- Women are also more at risk for developing an anxiety disorder, such as generalized anxiety disorder (GAD), panic disorder, and social anxiety disorder. This is both due to biological factors, like hormonal fluctuations and brain chemistry, as well as social factors, such as discrimination and violence.
- Although men are more likely than women to die by suicide, women report attempting suicide more often than men.
- The suicide rate for women in the U.S. is highest for women between the ages of 45-64. It is lowest among girls ages 10-14 and women 75 and older.
- Women who earn a lower income, have a history of trauma, and/or have been incarcerated are at a higher risk for suicide.
Finding effective medication and therapy options are important parts of treating depression. Certain types of depression are unique to women depending on their stage of life. For this reason, it is important to consider these hormonal and life changes when treating depression in women.
Fortunately, clinical depression is a very treatable condition. Sixty-five percent of people with depression will have a full remission of the disorder with effective treatment.
Resources from MHA
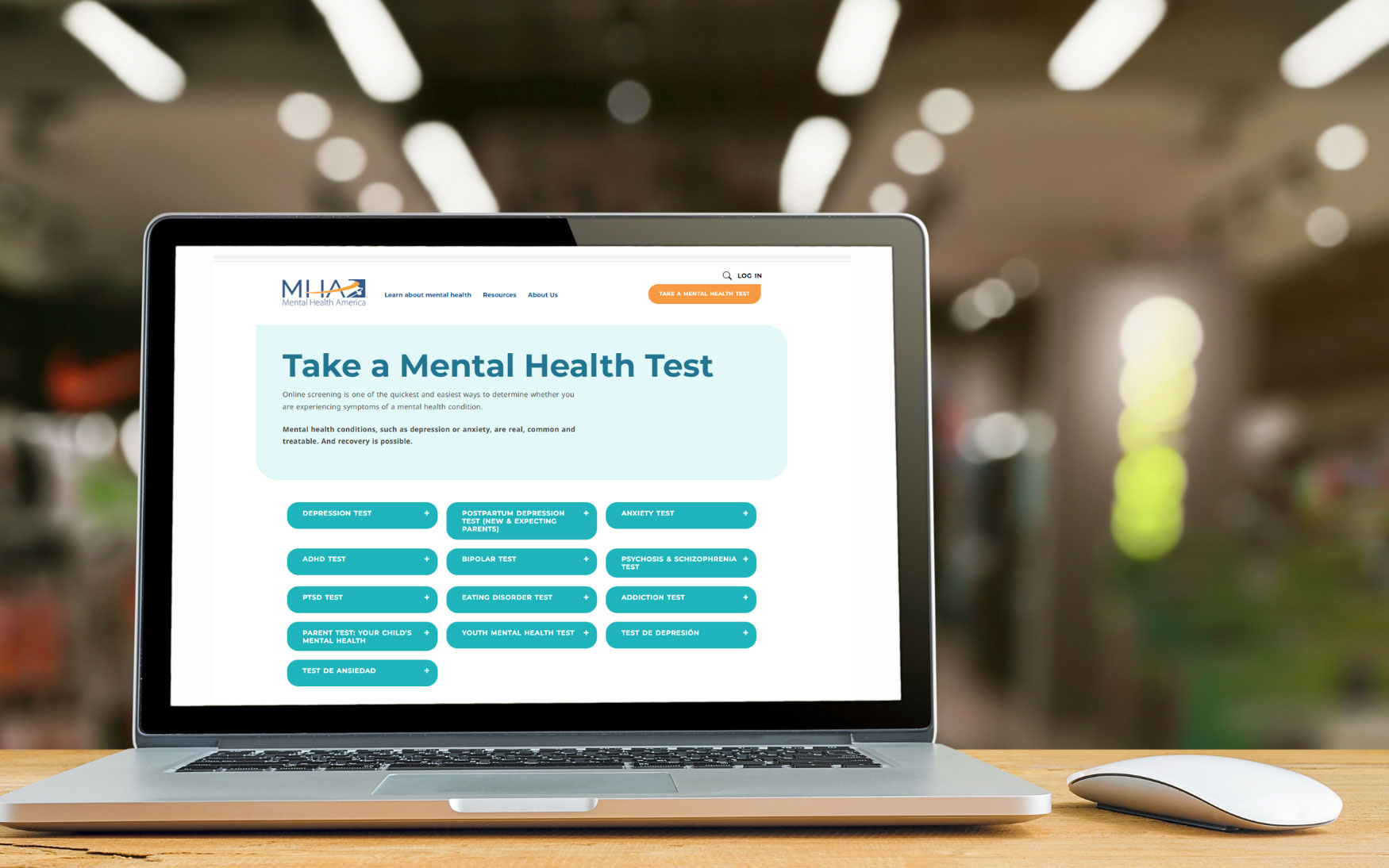
Take a Mental Health Test
If you are a new or expecting parent struggling with your mental health, you can take this Postpartum Depression Test or another mental health test at mhascreening.org. These mental health tests are anonymous, free, and private. It only takes a few minutes, and after you are finished you will be given information about the next steps you should take based on the results.
If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org. You can also reach Crisis Text Line by texting HOME to 741741.
This content created with support from Sage Therapeutics and Biogen.