The Mental Health of Healthcare Workers in COVID-19

If you are a healthcare worker and are concerned about your mental health, go to mhanational.org/frontline to be screened and find resources and support. If you are experiencing a mental health crisis, call 1-800-273-TALK (8255) to reach a 24-hour crisis center, or text MHA to 741741 to reach a trained Crisis Counselor 24/7.
Throughout the COVID-19 pandemic, Mental Health America (MHA) has witnessed increasing numbers of anxiety, depression, loneliness, and other mental health concerns. COVID-19 has had a profound negative effect on the mental health of the nation, especially among those who are faced with combating the virus.
While many throughout the U.S. are coping with the fear and uncertainty of COVID-19 from their homes, essential workers, including healthcare workers, must expose themselves to the virus every day. Healthcare workers are also experiencing conditions that have been compared to a war zone, continuously witnessing the direct effects of the pandemic as it spreads throughout communities. It is essential that we provide resources to help healthcare workers cope with the mental health impact of their work.
From June-September 2020, MHA hosted a survey on mhascreening.org to listen to the experiences of healthcare workers during COVID-19 and to create better resources to help support their mental health as they continue to provide care.
The responses collected from the 1,119 healthcare workers surveyed indicated that they are:
- Stressed out and stretched too thin: 93% of health care workers were experiencing stress, 86% reported experiencing anxiety, 77% reported frustration, 76% reported exhaustion and burnout, and 75% said they were overwhelmed.
- Worried about exposing loved ones: 76% of healthcare workers with children reported that they were worried about exposing their child to COVID-19, nearly half were worried about exposing their spouse or partner, and 47% were worried that they would expose their older adult family member(s).
- Emotionally and physically exhausted: Emotional exhaustion was the most common answer for changes in how healthcare workers were feeling over the previous three months (82%), followed by trouble with sleep (70%), physical exhaustion (68%) and work-related dread (63%). Over half selected changes in appetite (57%), physical symptoms like headache or stomachache (56%), questioning career path (55%), compassion fatigue (52%) and heightened awareness or attention to being exposed (52%). Nurses reported having a higher exposure to COVID-19 (41%) and they were more likely to feel too tired (67%) compared to other healthcare workers (63%).
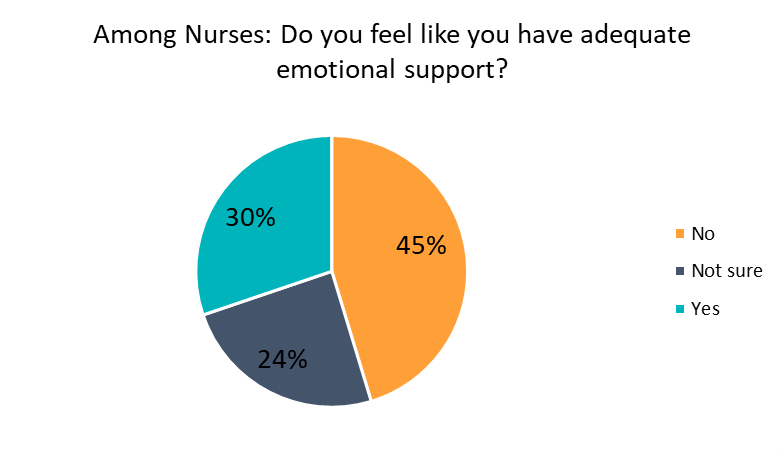
- Not getting enough emotional support: 39% of healthcare workers said that they did not feel like they had adequate emotional support. Nurses were even less likely to have emotional support (45%).
- Struggling with parenting: Among people with children, half reported they are lacking quality time or are unable to support their children or be a present parent.
Demographics
The following analysis is based on the responses of 1,119 healthcare workers surveyed on MHA Screening (mhascreening.org) from June 1-September 1, 2020.
The majority (76 percent) of respondents were young adults ages 18-44.
|
Age |
Count |
Percentage |
|
18-24 |
241 |
21.54% |
|
25-34 |
354 |
31.64% |
|
35-44 |
258 |
23.06% |
|
45-54 |
136 |
12.15% |
|
55-64 |
101 |
9.03% |
|
65+ |
29 |
2.59% |
|
Grand Total |
1,119 |
100.00% |
Most (70 percent) of the respondents were White, followed by Black or African American (10 percent), and Hispanic or Latino (8 percent).
|
Race/Ethnicity |
Count |
Percentage |
|
White (non-Hispanic) |
778 |
69.53% |
|
Black or African American (non-Hispanic) |
113 |
10.10% |
|
Hispanic or Latino |
88 |
7.86% |
|
Asian or Pacific Islander |
65 |
5.81% |
|
More than one of the above |
47 |
4.20% |
|
Other |
18 |
1.61% |
|
Native American or American Indian |
10 |
0.89% |
|
Grand Total |
1,119 |
100.00% |
The largest groups of respondents were other healthcare staff (30 percent) and nurses (22 percent). Nineteen percent of respondents identified their position as “Other,” which included mental health professionals, social workers, and pharmacy staff, among others.
|
What is your title or position? |
Count |
Percentage |
|
Other patient care (CAN, lab technician, X-ray, therapist, front desk, etc.) |
335 |
29.94% |
|
Nurse |
245 |
21.89% |
|
Other |
207 |
18.50% |
|
Community-based healthcare workers |
89 |
7.95% |
|
Doctor |
81 |
7.24% |
|
Support staff (janitor, food service staff, administrative, etc.) |
81 |
7.24% |
|
EMT/Paramedic |
50 |
4.47% |
|
Physician’s Assistant or Nurse Practitioner |
31 |
2.77% |
|
Grand Total |
1,119 |
100.00% |
Fifty-two percent of healthcare workers surveyed did not have direct known exposure to COVID-19 patients but had the potential for exposure. Twenty-eight percent were working directly with COVID-19 patients.
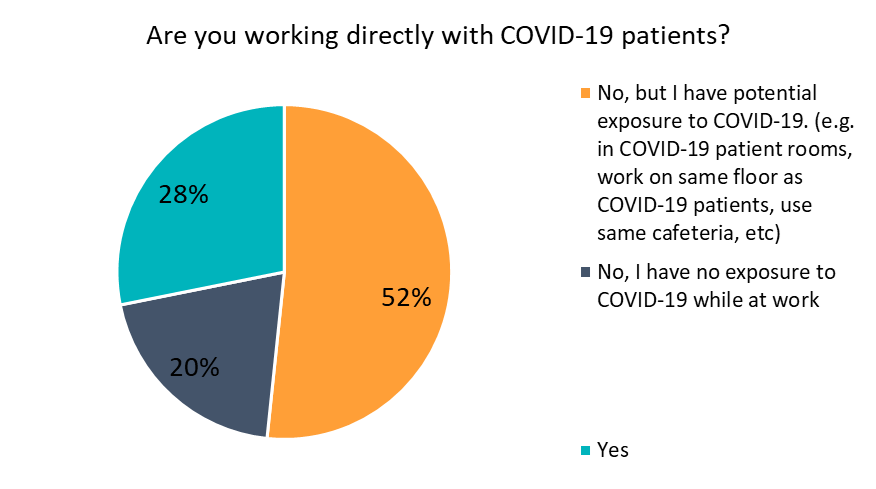
Nurses were more likely to report having exposure to COVID-19 patients than the general population of healthcare respondents. Among nurses, 41 percent reported they were working directly with COVID-19 patients, and 49 percent reported they had potential exposure.
|
Among Nurses: Are you working directly with COVID-19 patients? |
Count |
Percentage |
|
No, but I have potential exposure to COVID-19. (e.g. in COVID-19 patient rooms, work on same floor as COVID-19 patients, use same cafeteria, etc.) |
119 |
48.57% |
|
Yes |
100 |
40.82% |
|
No, I have no exposure to COVID-19 while at work |
26 |
10.61% |
|
Grand Total |
245 |
100.00% |
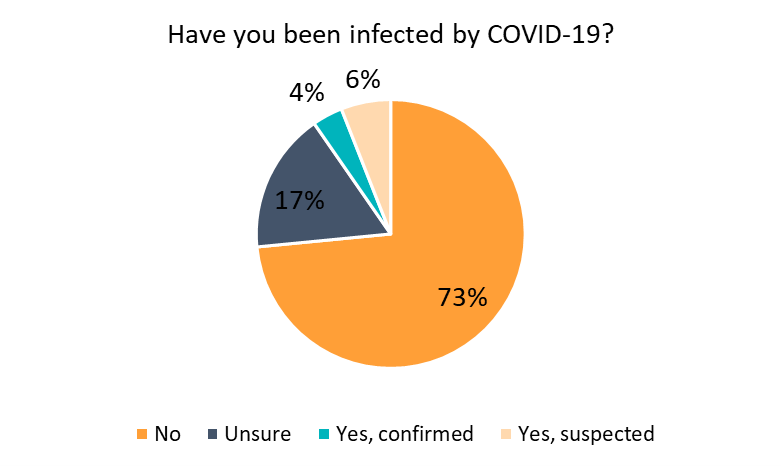
However, most (73 percent) respondents to the Healthcare Workers survey had not previously contracted COVID-19 at the time of surveying. 10 percent either had confirmed or suspected cases of COVID-19, and 17 percent were unsure.
Experiences of Healthcare Workers During COVID-19
MHA asked healthcare workers, “In the last three months, which of the following feelings have you been regularly experiencing? Check all that apply.”
Stress was the most commonly reported feeling, with 93 percent of healthcare workers indicating that they had regularly experienced stress in the last three months. This was followed by anxiety (86 percent), frustration (77 percent), exhaustion or burnout (76 percent), and feeling overwhelmed (75 percent). Gratitude, hope, and pride were reported by fewer people, although nearly a third (31 percent) reported that they regularly felt gratitude.
|
In the last three months, which of the following feelings have you been regularly experiencing? Check all that apply. |
Count |
Percentage |
|
Stress |
1038 |
92.76% |
|
Anxiety |
963 |
86.06% |
|
Frustration |
861 |
76.94% |
|
Exhaustion/Burn-out |
850 |
75.96% |
|
Overwhelmed |
844 |
75.42% |
|
Sadness |
751 |
67.11% |
|
Unappreciated |
670 |
59.87% |
|
Anger |
631 |
56.39% |
|
Fear |
618 |
55.23% |
|
Loneliness |
611 |
54.60% |
|
Powerless |
566 |
50.58% |
|
Disconnected |
552 |
49.33% |
|
Grief |
374 |
33.42% |
|
Gratitude |
347 |
31.01% |
|
Hope |
310 |
27.70% |
|
Pride |
220 |
19.66% |
MHA also asked healthcare workers, “In the last three months, have you experienced an increase in any of the following? Check all that apply.”
Healthcare workers were most likely to report that they had increases in emotional exhaustion in the last three months (82 percent). This was followed by trouble with sleep (70 percent), physical exhaustion (68 percent), and work-related dread (63 percent). Over half of healthcare workers also reported experiencing changes in appetite (57 percent), physical symptoms like headache or stomachache (56 percent), questioning their career path (55 percent), compassion fatigue (52 percent), and heightened awareness, worry or attention to being exposed (52 percent).
|
In the last three months, have you experienced an increase in any of the following? Check all that apply. |
Count |
Percentage |
|
Emotional exhaustion |
919 |
82.13% |
|
Trouble with sleep (difficulty falling or staying asleep) |
785 |
70.15% |
|
Physical exhaustion |
764 |
68.28% |
|
Work-related dread |
703 |
62.82% |
|
Change in appetite (overeating or undereating) |
634 |
56.66% |
|
Physical symptoms - headache, stomachache, etc. |
623 |
55.67% |
|
Questioning career path |
617 |
55.14% |
|
Compassion fatigue |
584 |
52.19% |
|
Heightened awareness/worry/attention to being exposed |
580 |
51.83% |
|
Lower self-esteem |
499 |
44.59% |
|
Upsetting thoughts, images and/or dreams |
475 |
42.45% |
|
Racing thoughts |
452 |
40.39% |
|
More likely to smoke, drink, and/or use substances |
430 |
38.43% |
Emotional Support for Healthcare Workers
When asked about emotional support, the largest group (39 percent) of healthcare workers indicated that they did not feel they had adequate emotional support. Another 26 percent were unsure if they were receiving adequate emotional support.
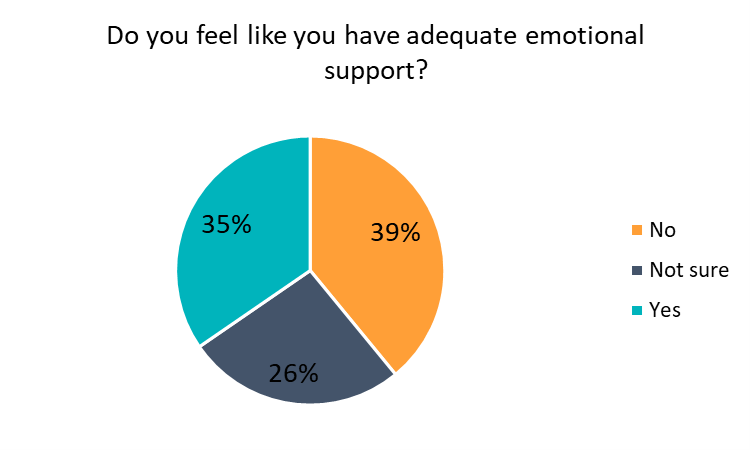
Nurses were even less likely to report that they had adequate emotional support than other healthcare workers. Among the nurses surveyed, 45 percent reported that they did not have adequate emotional support and 24 percent were not sure.
Over half of healthcare workers were receiving emotional support from family (57 percent) and friends (53 percent). Many healthcare workers also reported receiving emotional support from their same-level coworkers (38 percent).
|
From whom do you receive emotional support? Check all that apply. |
Count |
Percentage |
|
Family |
634 |
56.66% |
|
Friends |
593 |
52.99% |
|
Significant other |
437 |
39.05% |
|
Same level co-workers |
430 |
38.43% |
|
Supervisor |
171 |
15.28% |
|
Therapist |
169 |
15.10% |
|
No one |
136 |
12.15% |
|
Support group (live virtual group or social media group) |
57 |
5.09% |
|
Roommate(s) |
41 |
3.66% |
|
Other |
33 |
2.95% |
Work-Related Stressors
When asked to select their top three work-related stressors, 61 percent reported uncertainty about when things will settle down or return to normal, and 54 percent reported experiencing burnout. Nearly half (49 percent) also reported that their heavy or increased workload was a major stressor in the previous three months.
|
What are your top three work-related stressors over the last three months? Check all that apply. |
Count |
Percentage |
|
Uncertainty about when things will settle down/return to normal |
678 |
60.59% |
|
Burnout |
599 |
53.53% |
|
Heavy/increased workload |
544 |
48.61% |
|
Concern of getting sick myself |
484 |
43.25% |
|
Concern of spreading COVID-19 |
396 |
35.39% |
|
Insufficient communication from leadership |
337 |
30.12% |
|
Insufficient PPE |
289 |
25.83% |
|
Working too many hours |
271 |
24.22% |
|
Job security/employment status |
253 |
22.61% |
|
Insufficient training |
142 |
12.69% |
|
Distress about how to effectively treat COVID-19 patients |
136 |
12.15% |
|
Inappropriate role designation |
127 |
11.35% |
|
Working at a new location |
121 |
10.81% |
|
Witnessing high number of deaths |
101 |
9.03% |
|
Other |
55 |
4.92% |
|
Treating coworkers with COVID-19 |
29 |
2.59% |
Fear of Exposure and Increased Stress at Home
Most healthcare workers reported that they were worried about exposing the people they lived with to COVID-19. Forty-seven percent reported being worried about exposing their older adult family, and 45 percent were worried about exposing their spouse or partner. Seventy-six percent of healthcare workers with children reported they were worried about exposing their children. Nearly half (45 percent) selected more than one option.
|
Are you worried about exposing the people you live with to COVID-19? If yes, who? Check all that apply. |
Count |
Percentage |
|
Exposing my child |
358 |
75.80%* |
|
Exposing my older adult family |
521 |
46.56% |
|
Exposing my spouse or partner |
509 |
45.49% |
|
I'm not worried about exposing my household members |
170 |
15.19% |
|
I live alone |
158 |
14.12% |
|
Exposing my roommate |
111 |
9.92% |
*Percent determined from the number of respondents who reported having children, as opposed to the whole population of respondents.
When asked about their top three home-related stressors, the majority of respondents (63 percent) reported that they were too tired when they got home from work to do home-related tasks such as cooking and chores. Nurses were even more likely to report feeling too tired after work than other healthcare workers (67 percent). Forty-one percent of healthcare workers reported loneliness as a significant stressor, and over 40 percent reported financial stress.
Among healthcare workers who indicated that they had children, 34 percent indicated that not being able to support children or be a present parent was a major stressor, and 32 percent reported a lack of quality time with their children as a result of COVID-19.
|
What are your top three personal/home-related stressors over the last three months? |
Count |
Percentage |
|
I am too tired when I get home to cook, do chores, etc. |
700 |
62.56% |
|
Loneliness |
464 |
41.47% |
|
Financial stress |
453 |
40.48% |
|
Worry and/or guilt about infecting household members |
410 |
36.64% |
|
Taking stress out on my family |
384 |
34.32% |
|
Lack of quality time with partner(s) |
341 |
30.47% |
|
My partner doesn't understand the stress I'm under |
279 |
24.93% |
|
Inconsistent work hours/coordinating schedules |
262 |
23.41% |
|
Other family member(s) needing to take over my responsibilities |
112 |
10.01% |
|
|
|
|
|
Among people who reported having children: |
|
|
|
Being able to support children/being a present parent |
150 |
34.25% |
|
Lack of quality time with children |
142 |
32.42% |
|
Homeschooling |
125 |
28.54% |
|
Childcare |
96 |
21.92% |
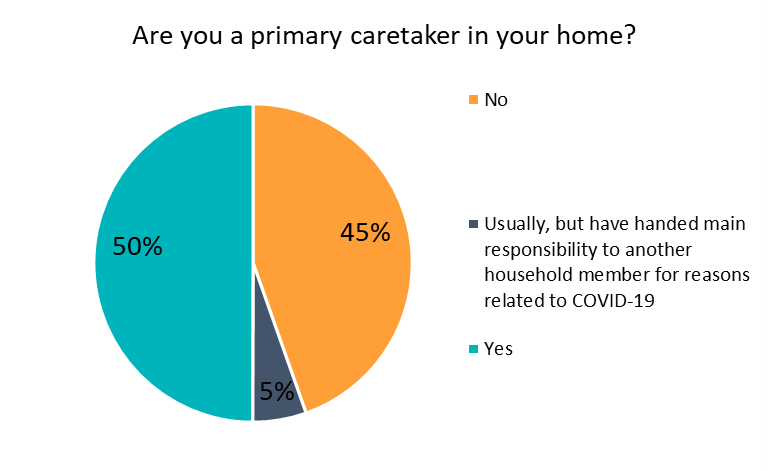
Half (50 percent) of healthcare workers indicated they were the primary caretaker within their homes. Another 5 percent normally would be the primary caretaker but had shifted responsibility as a result of COVID-19.
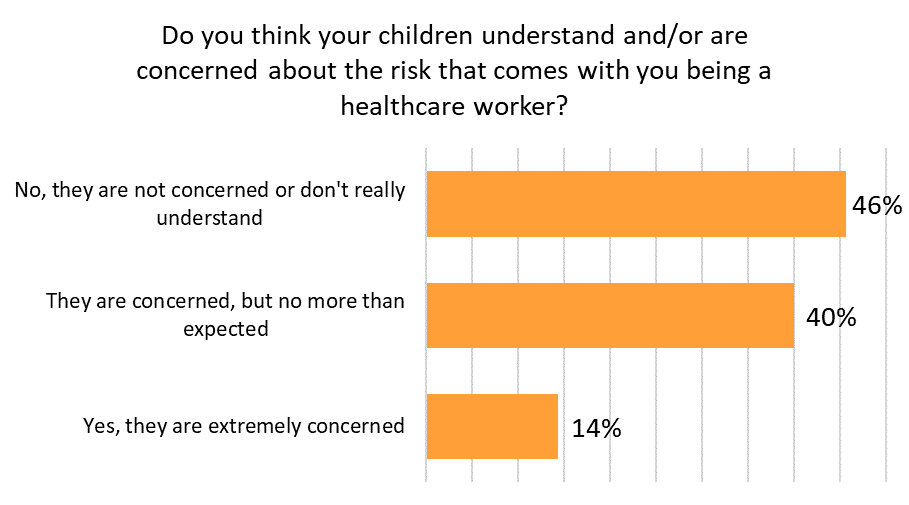
Among the healthcare workers who responded to this survey, 61 percent did not have children at home. However, among those who did report having children at home, 46 percent reported that their children either did not understand or were not concerned about them being a healthcare worker. Forty percent reported that their children were concerned but no more than expected, and 14 percent indicated that their children were extremely concerned.
For resources and supports for healthcare workers, please visit mhanational.org/frontline
The Healthcare Worker Survey was made possible by the generous support of the Johnson & Johnson Foundation.


