Pregnancy and the birth of a child can be a joyous and exciting time. But some people may struggle with depression as they transition to parenthood. Below you will find information, coping skills, and resources to support you through the challenges of postpartum depression.
The postpartum blues or "baby blues"
People who give birth often experience “the baby blues.” These are mood changes that are the result of hormonal fluctuations. They occur during and immediately after childbirth. Postpartum blues are very common. They usually start two to three days after delivery and typically subside as hormone levels begin to stabilize.
Symptoms generally do not last for more than a few weeks. The postpartum blues are not considered a mental health condition. If a person continues to experience mood swings or feelings of depression for more than two weeks after childbirth, it is important to see a medical professional.
What is postpartum depression (PPD)?
Postpartum depression (PPD) is a major form of depression. While it is less common than postpartum blues, it is estimated that 10 to 20 percent of new parents who have given birth experience PPD. PPD includes all the symptoms of depression, but occurs only following childbirth. It can begin any time after delivery and can last up to a year.
The medical community can play a key role in identifying and treating PPD. After giving birth, new parents should see their doctor to determine their risk for developing PPD. Early identification of parents who are at risk can enable them to seek support from physicians, partners, friends, and coworkers.
What are the symptoms of PPD?
Symptoms of PPD are similar to those of clinical depression, such as a loss of pleasure in things you typically enjoy or a loss of energy, but also include:
- Feeling like a bad parent
- Feelings of self-blame and guilt
- Feeling worried for no good reason
- Feeling hopeless or overwhelmed
- Excessive anxiety about the child’s health
- Intrusive thoughts of harming the baby or yourself
- Difficulty bonding with the baby
- Drastic changes in appetite or sleep
- Feeling like no one understands what you are going through
- Feelings of isolation and loneliness
Symptoms of PPD must be present for more than two weeks following childbirth to distinguish them from postpartum blues.
What factors contribute to PPD?
The following factors may contribute to the development of PPD:
Hormonal changes
A person experiences the greatest hormonal fluctuation levels after giving birth. The rapid drop in estrogen and progesterone after delivery can trigger a depressive episode because these hormones help regulate mood and anxiety.
Life stressors
If a major event like the death of a loved one or loss of a job happens during pregnancy, a parent may be more susceptible than average to PPD. Ongoing stressful circumstances may also trigger PPD. For example, stress at the office added to the responsibilities of being a parent can cause emotional strain that could lead to PPD. According to data from MHA’s screening tool, life stressors such as relationship challenges, financial hardship, loneliness, and poor self-image/body image also contribute to PPD symptoms.
Societal factors
Different demographic groups are at a higher risk for PPD. According to data from MHA’s screening tool, younger screeners ages 11-24 were the most at-risk age group for PPD. Parents from the LGBTQ+ community, especially transgender and non-binary individuals, are also at a higher risk for PPD. Multiracial and Indigenous communities are the racial/ethnic groups most at risk. Trauma survivors and parents with a lower household income are also more likely to experience PPD.
What treatments are available?
There are multiple treatment options available for PPD. Medication or therapy may be used alone or together. You can work with your care team to find the right combination of treatments that will be most effective for you.
Psychotherapy alone may also be used to treat PPD. New parents should be encouraged to talk about their feelings or fears with others.
Taking antidepressant medication may provide relief for PPD symptoms.
For those who choose to breastfeed/chestfeed, it is important to have discussions with your healthcare provider about medication options. Some medications pass through to milk in higher concentrations than others. Using a combination of breast/chest milk and formula, and taking medication at certain times can help minimize the amount that passes through to your baby.
New, fast-acting treatments are available for people with PPD. These medications are only taken for 14 days and can provide relief in as early as three days. Typical antidepressant medications can take several weeks before their effects are noticeable.
These new, fast-acting treatments do pass into breast/chest milk, so it is important to talk to your doctor about your options. You may be able to continue breastfeeding/chestfeeding for the 14 days you are on the medication, or you may decide to pause breastfeeding/chestfeeding after you are one week past your last dose. Together, you and your doctor can decide what will work best for you and your baby.
Does PPD affect babies?
When a new parent has severe depression, it may be harder for the parent and child to bond. You may be less able to respond to your child’s needs. Studies show that the more depressed a new parent is, the greater the delay in the infant’s development. But by doing your best to take care of yourself and reaching out for help when you need it, your child will be able to get the care and attention they need.
PPD and self-care
It can be challenging to find time to take care of yourself with a new baby to care for. You may not even feel like you have the time to take a shower or use the bathroom. But doing your best to take care of yourself in ways that feel doable will allow you and your baby to feel more balanced.
Reaching out for support
Socializing through support groups and with friends can play a critical role in recovery. Asking your support networks for help taking care of your baby can also give you the time and space to do the things you need to feel at ease. Sometimes, it can feel hard to reach out for help, but this support can go a long way in helping you and your baby get your needs met.
Movement
Regular movement can support a new parent’s recovery from PPD. Walking, running, swimming, dancing, and other movement-based activities release feel-good chemicals in the brain, such as dopamine. This can give you a mood-boost and increase feelings of motivation. Some activities also involve a social component, like postpartum yoga classes, where you can find additional opportunities for connection and support.
Nutrition
Studies show that eating a healthy diet in the postpartum period decreases the risk of experiencing PPD symptoms. Eating a balanced amount of fruits, vegetables, fish, grains, legumes, and herbs are especially helpful for supporting postpartum mental health. It may not always be easy to cook and go grocery shopping with a new baby at home. But reaching out for help from your support network and using services that make healthy-eating more accessible, like grocery delivery or healthy take-out options, can make it easier.
Sleep
Sleep disturbances and disorders can make PPD more challenging. Sleep is often interrupted for new parents because of breastfeeding/chestfeeding at night. But especially for people who are at a higher risk for PPD, protecting at least one, four-hour period of consolidated sleep has been effective in reducing PPD symptoms. Asking for help from your support network to help you with night-time feedings can allow you to get the rest you need. Also, while the loss of sleep that comes with being a new parent can be exhausting, do your best to be mindful of how much caffeine you are consuming as this can trigger anxiety and mood changes.
Managing stress
Doing whatever you can to reduce your stress can make this challenging time a bit easier. You can try practicing mindfulness meditation either by yourself or while holding your baby. Studies show that practicing mindfulness during pregnancy may reduce anxiety and depression during the postpartum period. Ask for support from others to watch your baby so you can do activities that bring you joy, such as spending time outside or engaging in a hobby. Having a crying infant in your home, especially if they are not able to be soothed, can be overwhelming. If you get to the point where the stress feels unmanageable, it is ok to place the baby in a safe space, like their crib, and step away for a couple minutes. This allows you the space and time to collect yourself rather than trying to deal with an upset child while your emotions are also running high.
Navigating PPD while adjusting to being a new parent can be a lot to manage. You may face feelings of inadequacy as a parent or total overwhelm as you try to handle your responsibilities each day. But remember that you are deserving of grace, compassion, support, and rest. Do your best to find ways to celebrate yourself for everything that you are doing to care for yourself and your baby during this difficult time.
Outside resources
The National Maternal Mental Health Hotline – 1-833-TLC-MAMA – is a free and confidential space for pregnant women and new moms to get the emotional and mental health support they need. Trained counselors are available 24/7 by phone and text in English, Spanish, and translation services in over 60 languages.
Policy Center for Maternal Mental Health
Health Resources and Service Administration: Maternal and Child Health
CDC Reproductive Health: Depression resources
Connecting Rainbows: Coming out and postpartum
Postpartum Support International
PSI: Queer and Trans Parent Support Group
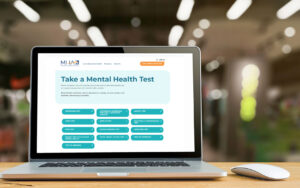
Take a mental health test
If you are a new or expecting parent struggling with your mental health, you can take this Postpartum Depression Test or another mental health test at mhascreening.org. These mental health tests are anonymous, free, and private. It only takes a few minutes, and after you are finished you will be given information about the next steps you should take based on the results.
If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org. You can also reach Crisis Text Line by texting HOME to 741741.